Let’s Talk About Gestational Diabetes
I’ve spent over 25 years helping women manage gestational diabetes mellitus before, during, and after pregnancy.
I’ve worked with hundreds of patients, trained other dietitians, and watched the same fears and struggles come up over and over.

If this is your first time hearing the words “gestational diabetes,” or if you’ve just been diagnosed, take a breath. You’re not alone, and this is manageable.
Up to 14% of pregnancies worldwide are affected by gestational diabetes each year.
It’s more common than most people realize, and being diagnosed doesn’t mean you’ve failed or done something wrong. It simply means your blood glucose levels are elevated during pregnancy and your body needs a different level of support right now.
Managing gestational diabetes starts with understanding how food, hormones, and lifestyle come together.
A healthy diet plays a major role in keeping your blood sugar stable, but it’s not the only piece. Working closely with your health care team; your OB, a registered dietitian, maybe even a diabetes educator can help you feel informed and supported every step of the way.
This isn’t about restriction or extreme dieting. It’s about building a plan that makes sense for your life. That includes learning how to balance your carbohydrate intake, eat in a way that works with your lifestyle and blood sugar patterns, while staying active in a safe, sustainable way.
In this post, I’ll walk you through:
- What gestational diabetes is and how it develops
- How nutrition, movement, and medication may play a role in managing it
- How to build meals that won’t spike your blood sugar
- What happens after delivery, and how to protect your long-term health
If you’ve been feeling overwhelmed, I want to help you feel more in charge. You can have a healthy pregnancy, even with gestational diabetes. And you don’t have to figure it out alone.
What Is Gestational Diabetes, Really?
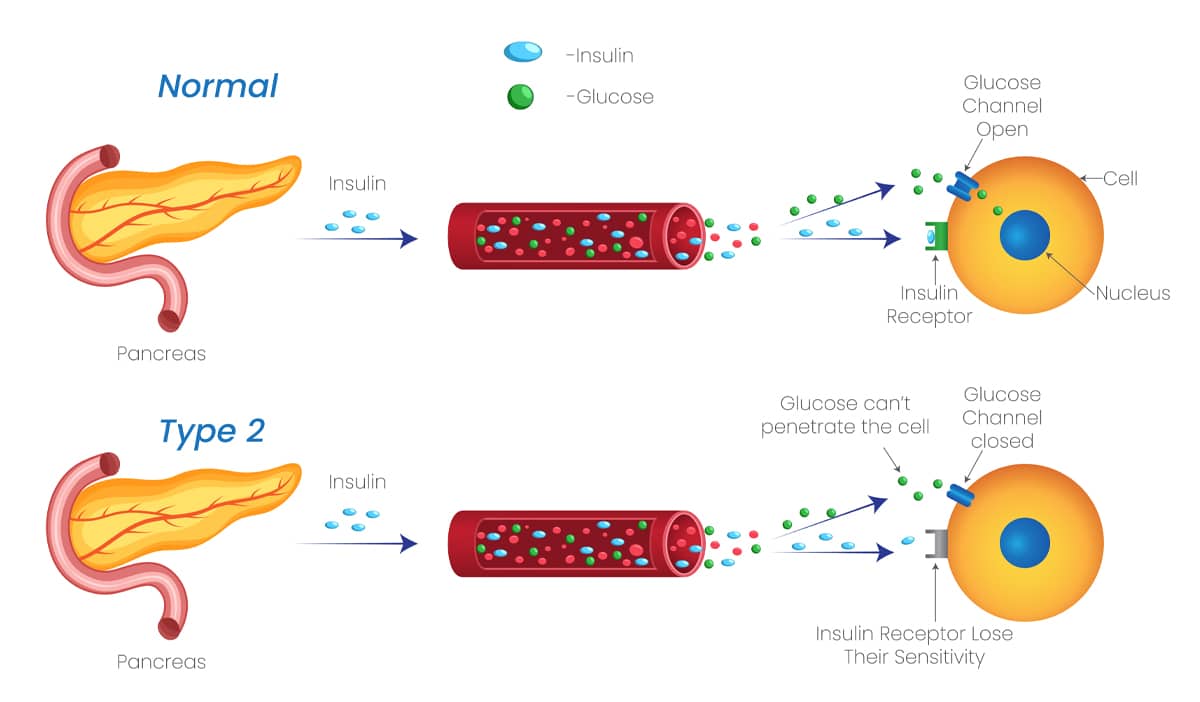
Gestational diabetes happens when your body doesn’t use insulin effectively during pregnancy. Insulin is the hormone that helps move sugar (glucose) from your bloodstream into your cells to be used for energy.
When insulin isn’t working well, due to the hormonal shifts that happen in pregnancy, blood glucose levels can rise too high. This leads to what we call gestational diabetes mellitus, or GDM for short.
Most cases are diagnosed between the 24th and 28th week of pregnancy. Some women develop it earlier, especially if they’re already at higher risk due to being overweight, obese, or having a family history of diabetes.
When you already have some degree of insulin resistance, the added strain of pregnancy hormones can push your blood sugar level out of the healthy range.
Even if you’re eating well, high blood glucose levels can still occur. And when they’re left unmanaged, it can lead to increased risk of complications. These may include delivering a larger baby, which can cause problems during labor, or early delivery due to high blood sugar levels affecting the pregnancy.
There’s also a higher chance of developing high blood pressure, preeclampsia, or needing a cesarean section. You are also at increased risk of developing Type 2 diabetes later in life if you’ve had GDM during a pregnancy.
The good news is, most cases of gestational diabetes are temporary. It usually resolves after the baby is born, but it should never be ignored. This diagnosis gives you the chance to act early and protect your long-term health.
In most cases, dietary changes and physical activity are enough to keep blood sugars under control. But some women may need insulin injections if lifestyle changes aren’t enough. That means your body needs a little more help to stay within target blood sugar levels and that’s ok.
With the right support and a realistic plan, you can have a healthy pregnancy and a healthy baby, even with gestational diabetes.

How a Gestational Diabetes Diet Supports Stable Blood Sugar Levels
When it comes to managing gestational diabetes mellitus, food is a major part of the equation, but it’s not the only part.
What helps keep blood sugar levels in a normal range is a combination of balanced nutrition, regular movement, and sometimes medication. Each one plays a role, and together they can make a real difference.
Even if you’re eating well and staying active, some women will still need medication.
Insulin resistance increases as pregnancy progresses due to hormonal shifts, especially in the third trimester. For some women, the body just needs more help and there’s no shame in that.
What you eat every day has a powerful effect.
The key is focusing on complex carbohydrates like whole grains and fiber-rich foods, as well as lean proteins and healthy fats. These nutrients work together to help slow digestion and stabilize your blood sugar level.
Instead of cutting carbohydrates completely, spread them out throughout the day and pair them with fat and protein. This approach helps your body process carbohydrates more gradually.

Skipping meals or severely restricting carbohydrates can actually lead to high blood sugar later in the day, along with fatigue, irritability, or cravings.
I also encourage women to pay close attention to sugar-sweetened beverages and sugary drinks like soda, sweet tea, and sports drinks like gatorade. These beverages contain the simplest forms of carbohydrates that can lead to spikes in blood sugar. Even 100% fruit juice, which sounds healthy, can cause quick blood sugar elevations because of the natural sugar it contains.
Reading food labels is also key to catching hidden sugars and spotting excessive amounts of simple carbohydrates in packaged foods. A quick rule of thumb when reading a food label is to make sure a product has less than 5% of the daily value or less in sugar. This is considered a LOW source of added sugars.
Don’t forget about dairy products. Getting enough calcium during pregnancy is important.
Many women ask if they can still enjoy yogurt or milk, and the answer is yes. I recommend choosing plain yogurt, since it doesn’t contain added sugars, always being mindful of portion sizes.
Both milk and yogurt contain carbohydrates, so it’s important to understand how they fit into your overall plan. Pairing them with protein or fiber can also help support more stable blood sugar levels.
What works for one woman may not work for another. That’s why personalizing your approach is key.
What matters most is finding the right balance of carbohydrates, protein, and fat that works for you.
Need help personalizing this?
Book a call with me and let’s build a pregnancy-friendly plan that actually works.

Blood Sugar Level Tips: Foods That Help, Foods to Avoid
When you’re following a gestational diabetes diet, the goal isn’t to eliminate carbohydrates, it’s to understand how and when to incorporate them into your diet. The key is learning how to space them out, pair them wisely, and keep an eye on portions.
Carbohydrates often get a bad reputation, especially in pregnancies with gestational diabetes, but they’re an essential part of a balanced diet. Instead of avoiding them completely, it’s more helpful to have a plan for how to include them in a way that supports stable blood sugar levels.
With the right combinations and timing, carbohydrates can absolutely be part of a healthy, nourishing routine.
Here are some foundational strategies I share with the women I work with:
Eat Regular Meals and Spread Out Carbohydrates
Skipping meals or loading up on carbohydrates all at once has the capacity to rapidly increase your blood sugar. Spacing meals and snacks throughout the day gives your body time to handle what you’ve eaten.
For most people, three meals a day and snacks as needed works well. But it’s not just about when you eat. What you eat with these carbohydrates matters just as much.
Carbohydrates Are Not the Problem. The Type and Amount Matter
It’s also helpful to minimize sugary foods and processed snacks, especially those with added sugar.
Treats like candy, pastries, sweetened yogurt, and flavored coffee drinks can cause a sharp rise in blood sugar levels. These foods can still fit in from time to time, but how often and how much matters.

Foods to Limit or Avoid
The foods below should be minimized or avoided if your blood sugar numbers are consistently high:
- Sugary drinks (juice, soda, sweet teas, sports drinks)
- White bread, bagels, crackers
- Granola bars or energy bars (many are high in sugar)
- Sugary breakfast cereals with added sugar
- Desserts and pastries
If you’re looking for a convenient option that won’t spike your blood sugar, ALOHA Bars are a smart alternative. They’re made with organic ingredients, plant-based protein, and no artificial sweeteners or sugar alcohols. ALOHA Bars can be a great on-the-go snack, especially when paired with fiber or healthy fat. If you’re curious, check them out here (affiliate link).
Note: I may earn a small commission if you purchase ALOHA Bars through the link provided. I only recommend products I genuinely trust and use in my practice at no extra cost to you.
If you’re ever unsure how a food affects your blood sugar, a registered dietitian (RD), like myself, is the best person to guide you. Your registered dietitian can help look at your blood sugar numbers and help you adjust your carbohydrates accordingly.
Some women are able to tolerate an amount of sugar in their diet and some can not depending on the amount of insulin resistance the woman is experiencing. Your health care team can help whether it’s adjusting carbohydrates or adding medication if needed. Remember, diet alone can not manage all blood sugar elevations.
As part of your care plan, you should be testing your blood sugar four times a day; once fasting, and again one hour after each main meal (breakfast, lunch, and dinner).
These numbers help us understand how your body is responding to different meals and portion sizes.
As your RD, my job isn’t just to help manage your blood sugar levels, it’s also to make sure you’re eating enough, maintaining energy, and not losing weight unnecessarily.
We review your food and glucose logs together and make adjustments that support both your health and your baby’s growth. You should never feel like you have to go hungry to stay in range. Managing gestational diabetes is about eating well, not eating less.
Following a gestational diabetes diet doesn’t have to mean eating bland meals or cutting out everything you love. It just means understanding your carbohydrate choices and how they fit in your overall meal. Your registered dietitian is well equipped to help you with that every step of the way!

Foods That Won’t Spike Blood Sugars Too Quickly
Below are examples of supportive foods that can be part of your gestational diabetes diet when eaten in appropriate portions and balanced with other nutrients.
But, be careful. Even the most nutrient-dense carbohydrates like sweet potatoes or black beans can spike your blood sugar level if you eat too much at once or without protein or fat to slow digestion. Balance is key.
Carbohydrate Foods
These are higher fiber carbohydrates that do not spike blood sugars.
- Sweet potatoes
- Lentils, beans, chickpeas
- Berries, apples, pears
- Whole grains (quinoa, oats, brown rice)
- Plain Greek yogurt and milk
- Non-starchy vegetables like zucchini, peppers, spinach, broccoli, cauliflower
Protein Foods
These help stabilize blood sugar levels, promote satiety, and support a healthy pregnancy.
- Eggs
- Chicken, turkey, lean beef
- Fish (watch mercury levels during pregnancy)
- Tofu and tempeh
- Nut butters
- Unsalted nuts and seeds
Healthy Fats
Fats help slow digestion and blunt blood sugar spikes. They also support hormone production and nutrient absorption.
- Avocado
- Extra virgin olive oil
- Chia seeds, flaxseeds
- Walnuts, almonds, pistachios
Portion size and balance matter. You can eat most of these foods as long as you’re pairing wisely and monitoring how your body responds. That’s why working with a registered dietitian to review your food log alongside your blood glucose readings is so important.
Want to track what you’re eating, how you’re feeling, and what’s working for your body? Download my Mindful Eating Journal here.

Managing Weight Gain During Pregnancy
Weight gain is expected during pregnancy. When you’re managing gestational diabetes, the rate and pattern of that gain matters. Gaining too much, too quickly can make blood sugar harder to control and increase the risk of complications.
In my practice, I don’t focus on strict numbers or calorie counting. Instead, I help my clients tune into what their bodies need, support steady weight gain, and avoid the spikes and crashes that come from inconsistent meals or unbalanced carbohydrate amounts.
If you’re not sure what’s appropriate for you, let’s talk. Together, we can look at your patterns, your meals, and your lifestyle to create a plan that keeps your blood sugar more stable and supports a healthy pregnancy.
You don’t need to be perfect, just consistent with the habits that make you feel good and keep your body working for you and your baby.
Eating for a Healthy Baby: How the Glycemic Index Can Help
If you’re managing pregnancy with gestational diabetes, your eating habits play a big role in supporting a healthy baby. One tool you might hear about is the glycemic index (GI), a scale that measures how quickly certain foods raise your blood sugar.
While I don’t rely on the glycemic index in my practice, it can be a helpful reference for some when choosing lower-impact carbohydrates.
The glycemic index can offer some insight, although it doesn’t always reflect how your body will respond to real meals. That’s because the score changes when foods are eaten in combination, which is almost always the case.
If you’re curious about GI, focus on low glycemic index foods like lentils, steel-cut oats, sweet potatoes, and non-starchy vegetables. These tend to digest more slowly and can support a steadier blood glucose response, especially when paired with protein, fiber, and healthy fats.

The Role of Exercise in Managing Blood Sugar
Food is just one part of managing gestational diabetes, movement matters too. Regular physical activity helps your body use insulin more effectively, which means it can actually lower blood glucose levels and keep them in a healthier range.
Even a short walk after meals can support better digestion and smoother blood sugar regulation. Prenatal yoga, swimming, or other gentle activities can be great options depending on your energy levels and what feels good for your body.
That said, exercise isn’t meant to be used as a quick fix or a way to “undo” a meal. Using movement solely to lower blood sugar at all costs, like walking multiple times a day just to keep your numbers down, can lead to unsustainable or obsessive patterns.
What matters most is building a consistent, balanced routine that supports your long-term health and fits into daily life without adding stress.
Talk to your health care provider about what’s safe for you during pregnancy, and remember: consistency is more important than intensity.
Meal Ideas for Blood Sugar and Balance
Now that we’ve covered the basics, let’s look at a simple visual tool I often use with clients to build balanced meals that support stable blood sugar throughout the day: the Plate Method.
Plate Method for Gestational Diabetes:
- 50% non-starchy vegetables
- 25% lean protein
- 25% higher-fiber carbohydrate

Breakfast
- Eggs scrambled with spinach and feta + slice of whole grain toast + avocado
- Plain Greek yogurt with berries, chia seeds, and a sprinkle of nuts
- A small bowl of oats with plant based milk plus crushed nuts or nut butter
Lunch
- Grilled chicken salad with mixed greens, cucumber, cherry tomatoes, olive oil dressing + small side of quinoa
- Turkey and avocado wrap on a whole wheat tortilla + raw veggie sticks
- Lentil soup packed with non-starchy vegetables + side salad + half an apple with peanut butter
Dinner
- Baked salmon + roasted Brussels sprouts + sweet potato wedges
- Stir-fry with tofu, broccoli, bell peppers, and brown rice
- Ground turkey and veggie stuffed bell peppers + side of roasted cauliflower with fruit for dessert
Snacks
- Hard-boiled egg + whole grain crackers
- Cottage cheese or ricotta + pear slices
- Apple + almond butter
- Hummus + raw carrots or bell pepper strips
Blood Sugar-Friendly Meal Formula:
Fiber + Protein + Fat + Carbohydrates + Color
Making sure protein, fat, and fiber are present at each meal is what keeps blood sugar in check and keeps you full longer.

After Giving Birth: Why Gestational Diabetes Support Still Matters
Once the baby arrives, it’s easy to shift all your attention to feedings, diaper changes, and sleep (or lack of it). Most people stop thinking about gestational diabetes the moment they’ve given birth, but this is actually when prevention matters most.
If you were diagnosed with gestational diabetes mellitus, it’s essential to schedule a follow-up glucose screening with your OB six weeks after delivery. This test checks whether your blood sugar levels have returned to a normal range or if they remain elevated, which could signal type 2 diabetes. Skipping this test means you could be living with undiagnosed diabetes without realizing it.
Even if your blood glucose levels go back to normal, you’re still at an increased risk of developing type 2 diabetes later in life.
This risk is higher for women with gestational diabetes, especially if they experienced excessive weight gain, needed insulin, or delivered via caesarean section. The good news is that you can take meaningful steps now to lower that risk.
Working with a registered dietitian after delivery can help you personalize your nutrition to support recovery, stable blood sugar, and long-term health.
That means eating regular, balanced meals that include complex carbohydrates, lean protein, healthy fats, and plenty of fiber. Spacing out your carbohydrate intake throughout the day and avoiding large spikes in blood sugar can help your body stay in balance.

These habits don’t just benefit you, they help support your baby’s growth and development if you’re breastfeeding.
Speaking of breastfeeding, your body still needs fuel. Producing breast milk requires extra energy, and skipping meals or undereating can affect both your blood sugar level and your milk supply.
If you’re planning to get pregnant again in the future, now is the time to focus on prevention.
Healthy eating, regular physical activity, and gradual weight loss after pregnancy can lower your chances of developing gestational diabetes again or being diagnosed with type 2 diabetes down the road.
Postpartum is also an emotional time. Many women feel pressure to “bounce back” quickly, but healing, physically and emotionally, takes time.
Practicing mindful eating, getting enough rest, and asking for support when needed are all part of staying grounded in this new phase.
You did the work during pregnancy to support a healthy baby. Now it’s time to take care of yourself, too.
If you had gestational diabetes and want to prevent type 2 diabetes after delivery, I can help.
Book a complimentary discovery call to talk through your goals and set yourself up for long-term health.

Mindset, Motivation, and Mindful Eating
It’s common to feel overwhelmed after being diagnosed with gestational diabetes. Many women feel guilt, frustration, or even fear. I’ve seen it over and over in my work, and I want you to know this isn’t your fault.
Gestational diabetes is not a punishment. It’s a sign that your body has more insulin resistance than usual during pregnancy. That’s something we can work with. Taking care of your nutrition, moving your body, managing your weight, and staying consistent with healthy habits can reduce your risk of developing type 2 diabetes in the future.
This is your opportunity to get curious about what your body needs, not to punish yourself or restrict everything.
One of the most effective tools I use with clients is mindful eating. That means noticing how you feel before and after meals, slowing down when you eat, and learning to respond to hunger and fullness cues.

Download your free Mindful Eating Journal here.
If you’re ready to take care of yourself in a way that feels sustainable, this is a great place to start.
Final Thoughts + Encouragement
Many women experience Gestational Diabetes during pregnancy. Gestational Diabetes can feel like a lot at first, but it’s something you can handle with the right tools and support.
You don’t need to overhaul your entire life or follow a strict diet or eating plan.
You just need a strategy that fits your needs and helps you stay consistent. I’ve worked with hundreds of women in this exact situation, and I know how to guide you through it.
If you’re looking for support, I’m here to help.
Whether you’re still pregnant or already in the postpartum phase, this is a good time to take care of your health in a way that works long term.
If you’re wondering what kind of difference the right support can make, here’s what one of my clients had to say:

“My health before this program was terrible. I would eat whatever I wanted and my gestational diabetes was out of control. This situation really worried me and I knew I had to do something about it.
As I began working with Voula, I noticed that I was better able to manage my blood sugars and weight during the pregnancy. I now have more energy, and I am making better choices that don’t stop me from living life the way I did before. It’s not easy to make these changes, but having Voula there has made a huge difference.
What I enjoyed the most about working with Voula is her ability to motivate me, her wisdom, and how she is able to connect with me as I continue on my journey. Voula is really good at making recommendations that are realistic and manageable. She also cares about my progress and has helped me make long lasting behavior changes.
I now feel confident about producing a healthy baby and creating healthy habits for myself and my family for life.
Thank you Voula!”
-Victoria Moscatel
You don’t need to overhaul your entire life or follow a strict diet or eating plan.
You just need a strategy that fits your needs and helps you stay consistent.
I’ve worked with hundreds of women in this exact situation, and I know how to guide you through it.Let’s take the next step together. Book your complimentary call or download your free mindful eating journal and get started today.




